What is gum disease?
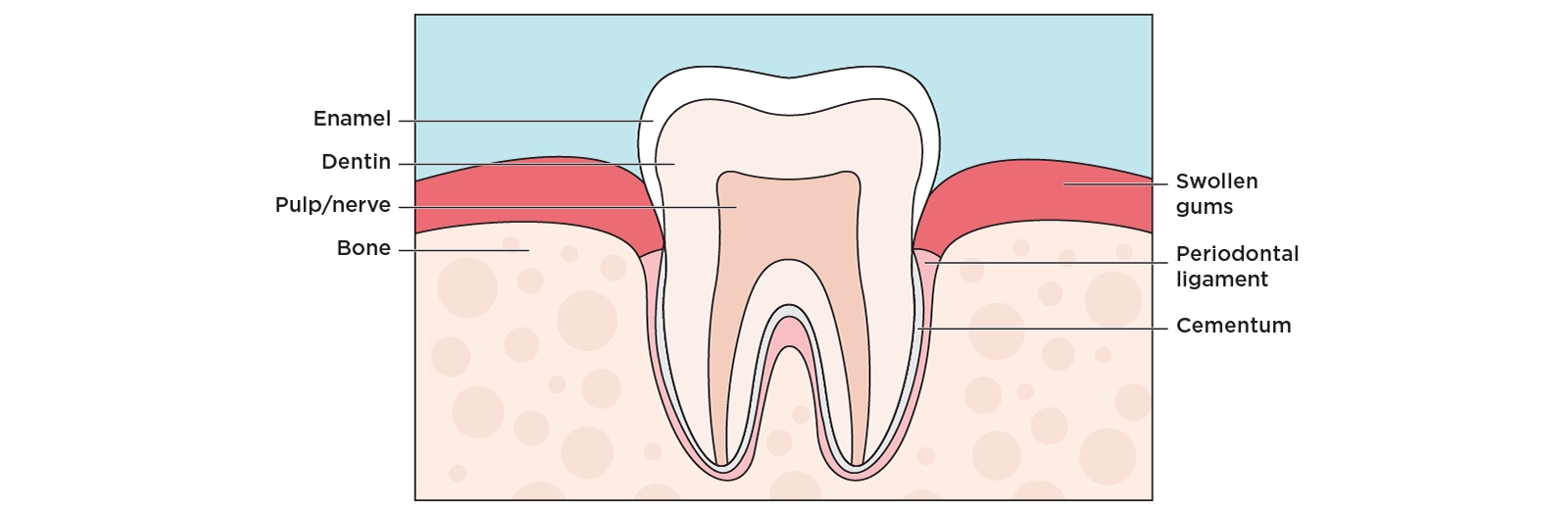
Gum disease refers to infections of the gum and bone tissues that surround your teeth. This kind of infection is also known by the technical names of gingivitis and periodontal disease.
Gum diseases are generally caused by poor oral health habits that allow a buildup of sticky, bacteria-filled plaque to accumulate on the teeth. If allowed to remain long enough, the bacteria releases toxins that infect the gum and eventually affect the bone supporting the teeth.
This infection typically causes irritation, redness and swelling along the gum line. If plaque is not removed from the teeth daily, then minerals in your saliva can transform that plaque into tartar. The presence of tartar can make it very difficult to clean your teeth properly and increase your likelihood of developing periodontal disease.
While improper oral health habits are a main cause of gum disease, a complex mix of genetic, systemic, local, and environmental factors also play a role in its development and progression.
Types of gum disease
There are two main types of gum disease. This includes:
Gingivitis
Gingivitis is the mildest form of gum disease and is usually the result of improper oral hygiene habits. While, typically, people experience very little or no discomfort, gingivitis causes inflammation of the soft tissue surrounding your teeth. Generally, your gums will become red, swell, and bleed easily. Gingivitis can be localized to one tooth or may affect the entire mouth.
The good news is, gingivitis is usually reversible. To remedy this infection, simply improve your oral health habits and at-home oral care routine. It is equally important to continue (or start) regularly visiting the dentist for professional cleanings as a dental professional can help to remove tartar that may be building upon your teeth and can help to identify early indicators of gum disease. It is important to note that, if left untreated, gingivitis can progress to a more serious form of gum disease, periodontitis.
Periodontitis
Periodontitis is a more advanced stage of gum disease in which the infection spreads beyond the gum line and irreversibly destroys the bone tissue that supports the teeth. During this process, gums become unattached from the tooth root and invading bacteria causes an inflammatory response that results in the destruction of gum tissue and the loosening of teeth from the bone. In some cases, periodontitis can also result in tooth loss.
Periodontitis is often categorized as mild, moderate, or severe, based on how much bone has been lost and if the inflammation is localized to one or more teeth or has spread throughout the mouth. When gum disease becomes this advanced, it becomes nearly impossible for an individual to clean their teeth properly below the gum line and professional care becomes necessary. Once you have progressed to periodontitis, continuous professional maintenance will always be required to prevent the disease from worsening.
Gum disease FAQs
-
What causes gum disease?
Gum disease is usually the result of improper oral hygiene, like improper and/or inconsistent brushing and flossing, which leads to a buildup of plaque on the teeth. Plaque then turns to tartar due to the minerals in your saliva, which, in turn, leads to the trapping of more plaque below the gum line. This then results in more inflammation along the gum line, as well as redness, tenderness, and sensitivity.
Other causes and influences on gum disease can include:
-
Smoking
-
Genetics
-
Diabetes and other systemic diseases
-
Stress
-
Crooked or grooved teeth that are not easily cleaned
-
Pregnancy, puberty, menstruation, other hormonal influences
-
Poor nutrition
-
Tooth grinding or clenching
-
Certain medications including steroids and oral contraceptives
-
-
Is gum disease reversible or curable?
Yes, when gum disease is in its mildest form, it can usually be reversed easily with better oral care. However, once gum disease has progressed far enough that it begins to destroy the bone and gum around the teeth, an ordinary cleaning is not enough to stop its progression.
If you have progressed beyond gingivitis to periodontitis, then you may need a procedure called periodontal scaling and root planning. This is more time-consuming and extensive than a routine cleaning but has the ability to remove tartar and plaque from the root surface that is causing the infection below the gum line.
Surgery may be recommended when deep pockets of infection persists after periodontal scaling. With surgical treatment, dental professionals can help correct defects by facilitating the growth of new, healthy gums and bone.
-
What is the difference between gingivitis and periodontitis
Gingivitis is a milder form of gum disease. With gingivitis the gums may become red, swollen, tender, or inflamed and may bleed easily. Gingivitis may or may not be painful and could be localized to just a couple of teeth or be a general issue throughout your mouth.
Without treatment, gingivitis can lead to periodontitis where the inflamed gum tissue starts to pull away from the teeth and form pockets. This can lead to greater infection, recession of the gums, pus, and will affect the bone that supports the teeth, leading to loose teeth or tooth loss.
-
What are the symptoms of periodontitis?
There are a number of indicators that gingivitis has progressed to periodontitis including:
-
Gum recession
-
Bone loss around your teeth
-
Loose or shifting teeth
-
Gums that separate from the tooth root and form deep pockets that are difficult, if not impossible, to clean
-
Pus filled gums
-
Sores in the mouth
-
Bad mouth odor
-
-
How can you prevent gum disease?
Luckily, when gum disease is in a milder form, it can usually be reversed by implementing better oral hygiene habits at home. Additionally, you can prevent its progression by:
-
Regularly seeing your dentist and receiving professional cleanings
-
Quitting smoking, if you smoke
-
Letting your dentist know of all systemic diseases you have, as well as, any prescription and over-the-counter medications that you take. Certain diseases and medications can cause gum inflammation or abnormal growth.
-
Following your dentist's recommendations for keeping your gums and teeth healthy
-
-
Can I catch periodontal disease from other people?
Most people probably don't realize it, but periodontal diseases are fostered by specific bacteria that we acquire from other people. However, research shows that you probably need to be susceptible in addition to being exposed to the bacteria.
Periodontal disease is sometimes passed from one family member to another. A 1997 article in the Journal of the American Dental Association states that the bacteria that cause periodontal diseases can be passed from person to person through saliva. Because of this, the American Academy of Periodontology recognizes that treating patients can sometimes involve treating several members of a family.
-
If my parents had periodontal disease, am I more likely to have it?
Genetics is a risk factor for periodontal diseases. Taking preventive steps, including routine oral care and preventive periodontal therapy, provides the best chance for good oral health.
Next steps after a gum disease diagnosis
If you’ve been diagnosed with gum disease, don’t wait, work with your dentist to create a treatment plan. With consistent care, many people can halt disease progression and protect their smile.
1. See a dental professional for a personalized treatment plan
If you have gingivitis or periodontitis, the first thing to do is schedule a follow-up with your dentist. Your provider will evaluate how advanced the disease is and recommend appropriate care, from deep cleaning to specialty referral.For more advanced disease, you may be referred to a periodontist (a gum specialist) for targeted therapy.
2. Professional treatments that might be recommended
Depending on severity, your dentist or periodontist may suggest:
-
Scaling and root planing (deep cleaning): This removes plaque and tartar from below the gumline and smooths root surfaces to help gums reattach.
-
Antibiotic therapy: Topical or oral antibiotics may be used to control bacterial infection.
-
Surgical options:
-
Flap/pocket reduction surgery
-
Bone grafts or guided tissue regeneration
-
Soft tissue (gum) grafts
These help repair structural damage and support healing in advanced cases.
-
3. Follow a strong oral hygiene routine at home
Treatment doesn’t end in the dental chair. Home care is critical to prevent disease from returning:
-
Brush 2–3 times daily, especially near the gumline.
-
Floss daily to remove plaque between teeth.
-
Use an antibacterial mouthwash if recommended.
-
Consider interdental brushes or water flossers for extra cleaning.
This combination helps break the cycle of bacterial buildup that drives gum disease.
4. Commit to regular follow-up and maintenance
Unlike simple gingivitis, periodontal disease often requires ongoing care even after treatment. Regular maintenance visits (sometimes every 3–6 months) help catch early signs of recurrence and keep gums healthy long-term.
5. Address lifestyle factors that affect gum health
Lifestyle changes can significantly support healing and prevention:
-
Quit smoking or tobacco use. Tobacco dramatically increases gum disease risk and limits healing.
-
Manage systemic health conditions like diabetes, which can affect gum disease progression.
-
Eat a balanced diet rich in anti-inflammatory nutrients (vitamins C, D, omega-3s) to support overall oral health. (Diet doesn’t replace dental care, but it can help reduce inflammation.)
6. Know when to seek immediate care
Contact a dental professional right away if you notice:
-
Increasing bleeding, swelling, or pus from gums
-
Pain that doesn’t improve
-
Loose teeth or changes in bite
-
Signs of infection after treatment
Gum disease doesn’t have to mean permanent damage. With professional treatment and the right daily habits, many people are able to manage the condition successfully. If you’re concerned about your gum health, reach out to your dentist for an evaluation and guidance on next steps. Understanding your options, and acting on them, is key to keeping your smile healthy for years to come.
Related Articles
Find a dental plan that is right for you
Find a Dental Plan